Prostate cancer is the most common cancer type in men, affecting nearly 11% of men in the U.S. Dr. Tewari is a prostate cancer expert, having completed more than 9,000 robotic prostatectomies in his career. Learn about how prostate cancer progresses and the treatment options across all stages of the disease.
What Is Prostate Cancer?
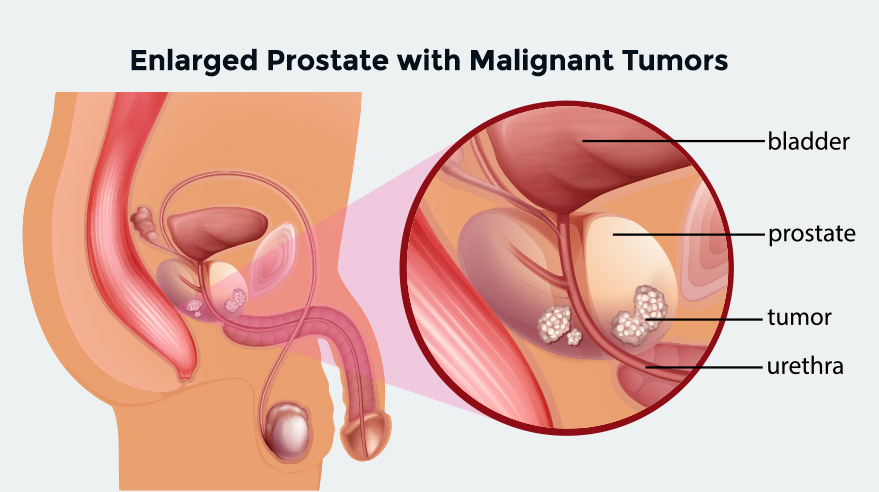
The prostate is a gland that is a part of the male reproductive system. Prostate cancer occurs when cells in the prostate gland grow and divide uncontrollably, forming a tumor. As men age, the prostate has a higher risk of developing cancer. It is a slow-growing cancer and may not cause symptoms in early stages.
The exact cause of prostate cancer is not yet fully understood. However, there are several factors that may contribute to the development of prostate cancer in men, including:
- Age
- Genetics
- Lifestyle factors
Symptoms of Prostate Cancer
Men with early-stage prostate cancer usually do not have noticeable symptoms. The first sign of the disease is often found during a routine screening exam. As the cancer progress, symptoms can include:
- Frequent urge to urinate
- Difficulty starting or holding back urination
- Weak or interrupted flow of urine
- Painful urination and ejaculation
- Blood in the urine or semen
- Difficulty having an erection
- Decreased fluid ejaculated
- Pressure or pain in the rectum
- Pain or stiffness in the lower back, hips, pelvis, or thighs
It is important to note that these symptoms overlap with other benign (non-cancerous) issues including enlarged prostate. Request an appointment if you have symptoms of prostate disease.

 International Patients
International Patients